best time to check blood sugar type 2 diabetes
Managing type 2 diabetes effectively requires a proactive approach, and one of the most critical tools in your arsenal is regular blood sugar monitoring. Knowing the best time to check blood sugar for type 2 diabetes is not a one-size-fits-all answer; it's a personalized strategy that provides a clear picture of how your body responds to food, medication, activity, and stress. This data empowers you and your healthcare team to make informed decisions about diet, exercise, and medication, ultimately helping to prevent complications and maintain long-term health. This guide will break down the optimal testing times, explain what the numbers mean, and help you build a monitoring routine that works for your life.
Understanding Your Blood Sugar Targets and Testing Times
Your doctor will set personalized blood sugar targets for you, typically measured in milligrams per deciliter (mg/dL). For most non-pregnant adults with type 2 diabetes, the American Diabetes Association (ADA) suggests general targets like a fasting blood sugar of 80-130 mg/dL and a post-meal level under 180 mg/dL. The timing of your checks is designed to see how well you are meeting these targets at different points in the day.
Here are the key times to check your blood sugar and why each is important:
- Fasting Blood Sugar (First thing in the morning, before food or drink): This is your baseline. It shows how well your body (and any long-acting medication) managed blood sugar overnight. A high fasting number can indicate the "dawn phenomenon" (a natural hormone surge) or insufficient medication.
- Before Meals (Preprandial): Checking before you eat gives you a starting point. It helps you understand how much a meal might raise your levels and can guide decisions about food portions or pre-meal insulin if prescribed.
- After Meals (Postprandial - 1 to 2 hours after starting a meal): This is a crucial check to see how your body responds to specific foods and meal sizes. The peak blood sugar impact typically occurs about 1-2 hours after eating. Keeping post-meal spikes under control is vital for managing your A1C.
- Before Bedtime: This check helps ensure you won't go too low (hypoglycemia) during the night, which can be dangerous. It's especially important if you take insulin or medications like sulfonylureas.
- Before, During, and After Exercise: Physical activity lowers blood sugar, but intense activity can sometimes cause a later spike. Testing around exercise helps you fuel safely and avoid lows.
- When You Feel Unwell or Stressed: Illness and stress hormones can significantly raise blood sugar. Monitoring during these times is essential.
Creating Your Personalized Blood Sugar Testing Schedule
Your testing frequency and focus depend largely on your treatment plan and how well your diabetes is managed. Work with your doctor or diabetes educator to design a schedule that provides meaningful information without causing burnout.
- If You Manage with Diet and Exercise Alone: You may start with less frequent testing, such as fasting checks a few times a week and occasional post-meal checks to see the impact of different foods.
- If You Take Non-Insulin Medications (e.g., Metformin): Your doctor might recommend a routine like checking fasting levels daily and rotating post-meal checks after different meals (e.g., after breakfast on Monday, after lunch on Tuesday).
- If You Take Insulin: More frequent testing is usually required—often before all meals and snacks, at bedtime, and occasionally during the night. This is necessary to dose insulin accurately and prevent hypoglycemia.
- When Your Routine Changes or A1C is High: If your numbers are not on target or you're starting a new medication, you may need a more intensive "testing profile." This often involves checking four or more times a day (fasting, before lunch, before dinner, bedtime) for a period to gather detailed data.
- Using Continuous Glucose Monitors (CGMs): For many, a CGM is a game-changer. This wearable device provides real-time glucose readings and trends 24/7, showing exactly how your levels fluctuate. It highlights highs and lows that fingerstick checks might miss and is excellent for understanding the impact of specific foods and activities.
Choosing the Right Tools and Interpreting Your Numbers
Having reliable equipment and knowing what to do with the numbers are the final, critical steps.
Essential Tools:
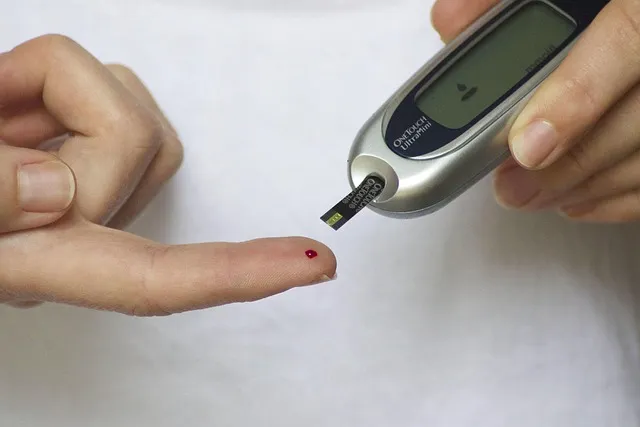
- Blood Glucose Meter (Glucometer): Choose one that is accurate, easy to use, and fits your budget (test strips are an ongoing cost). Many sync with smartphone apps for easy tracking.
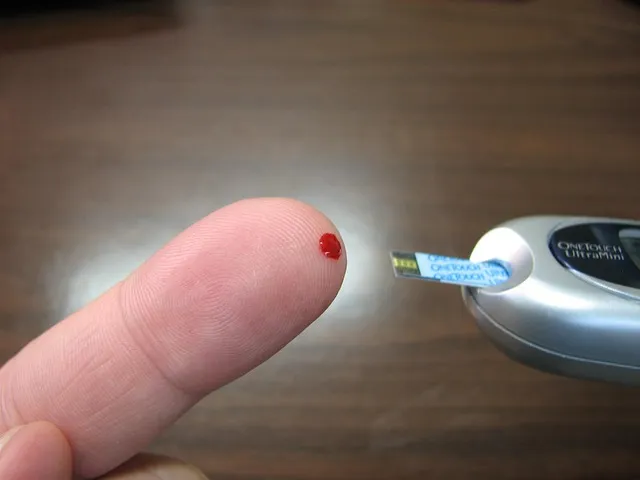
- Lancet Device and Lancets: Used to prick your finger for a small blood sample.
- Test Strips: Must be specific to your meter and stored properly.
- Logbook or App: Consistently recording your numbers, along with notes on food, medication, and activity, is key to spotting patterns.
What Your Numbers Are Telling You: Don't just collect numbers—analyze them. Look for patterns. Are your fasting numbers consistently high? Do certain meals, like pasta or pizza, cause larger spikes than others? Do your levels drop too low every afternoon after your walk? Bring this logged information to your medical appointments. It transforms your care from guesswork to data-driven decision-making, allowing your doctor to tailor your therapy precisely.

Frequently Asked Questions (FAQ)
Q: How often should I really be checking my blood sugar? A: There's no universal number. It depends on your treatment plan, stability, and goals. It could range from a few times a week to 6-10 times a day. Your healthcare provider will give you a personalized prescription for testing frequency.
Q: Is checking after meals really necessary if my fasting sugar is good? A: Yes, absolutely. Many people can have normal fasting glucose but experience significant spikes after eating. These post-meal spikes contribute directly to your average A1C level and can damage blood vessels over time.
Q: What should I do if my reading is unexpectedly high or low? A: Follow your personalized sick-day or hypoglycemia action plan from your doctor. For a high reading, drink water, take a walk if you feel able, and ensure you took your medication. For a low reading (typically under 70 mg/dL), follow the "15-15 Rule": consume 15 grams of fast-acting carbs (e.g., 4 oz juice), wait 15 minutes, and recheck. Repeat if still low. Always inform your doctor of recurring unexpected readings.
Q: Are fingersticks the only option now? A: No. Continuous Glucose Monitors (CGMs) are increasingly popular and covered by many insurance plans. They use a tiny sensor under the skin to read glucose levels in interstitial fluid, sending data to a receiver or smartphone every few minutes. They are ideal for seeing trends and preventing highs and lows.
Q: Does the time of day I take my medication affect when I should test? A: Critically yes. For example, if you take a rapid-acting insulin before meals, you must test before that meal to calculate the dose. If you take a long-acting insulin at night, a bedtime check is crucial. Always align your testing with your medication schedule as directed.
Conclusion
Determining the best time to check blood sugar for type 2 diabetes is about building a strategic window into your body's daily rhythms. By testing at key moments—fasting, before and after meals, and at bedtime—you gather the intelligence needed to manage your condition proactively. Remember, the goal is not just to collect numbers but to identify patterns, understand the effects of your lifestyle choices, and partner effectively with your healthcare team. With a consistent, personalized monitoring schedule and the right tools, you can take confident control of your blood sugar and pave the way for a healthier future with diabetes.
Related Articles

best time to take blood pressure medicine

best time to take turmeric for inflammation

best time to check blood sugar in the morning

when is the best time to take blood pressure medication

best time to take turmeric for weight loss
